How Do Hospitals Keep Their Air Clean
Source and pathway management should involve airborne transmission and particularly enhanced methods of its command even though the primary route is considered to be direct contact
Much attending is focused today on pathogenic microorganisms that accept developed resistance to antibiotic treatment, or entire types or classes of antibiotics. The loss of constructive antibody handling undermines the power of healthcare professionals to fight infectious diseases and manage their complications among immunocompromised patients.
The Centers for Disease Command and Prevention (CDC) estimates that more than ii one thousand thousand people in the United States are sickened every twelvemonth with antibiotic-resistant infections, with at least 75,000 dying (2013) as a result. Healthcare associated infections (HAIs) impale more people in this country than AIDS, breast cancer and auto accidents combined.
Healthcare associated infections are as well known as nosocomial infections or infirmary-acquired infections. They are transmitted by a diverseness of vectors, including person-to-person, through injection/insertion of medical devices, airborne contact of open wounds, and by respiration of airborne particles. Some emerging diseases, such as Middle East Respiratory Syndrome (MERS) are not all the same understood well enough to positively identify the transmission vector.
The most unsafe HAI pathogens are those that have the potential to spread past the airborne route (Kowalski 2006). Many of these pathogens, such as Methicillin-resistant Staphylococcus aureus (MRSA), are at present chosen "superbugs" because they are well-nigh invincible to standard drug treatments. Favorable indoor environments tend to self-perpetuate these agents, calculation to the concern by infection control specialists everywhere.
According to the CDC and World Health Organisation, antibody-resistant HAIs are on the rise. Support for airborne disease manual is likewise on the ascension (Fletcher et al. 2003). Evidence exists for airborne nosocomial transmissions of Acinetobacter, Pseudomonas, and MRSA (Allen and Green 1987), (Ryan et al. 2011) and (Farrington et al. 1990), and airborne manual tin can spread quickly and pervasively through a non-immune population (Weinstein 2004).
If mechanical and functional operations have remained unchanged, other sources of drug-resistant contamination must exist, presumably associated also with allusive paths of transmission. Therefore, source and pathway direction should involve airborne manual and especially enhanced methods of its control even though the primary route is considered to be direct contact. This article discusses several control methods.
Infection controls
Addressing infection control in hospitals requires integrating HVAC and air-pressure-control with dedicated infection-control systems, and minimizing unplanned airflows through building envelopes and interior spaces. Information technology besides benefits from the application of ultraviolet UV-C equipment from what is typically referred to in the healthcare industry (and the CDC) as ultraviolet germicidal irradiation (UVGI).
In that location are 4 methods used to reduce the concentrations of airborne infectious agents: dilution, filtration, pressurization, and disinfection. Following is a brief word of each method, with a focus on disinfection.
Dilution
Dilution ventilation helps to control infectious particles by introducing outdoor air, usually 2 to five air changes/hour (ACH), to dilute space air and so exhausting that amount as contaminated air. If 100 percent of all supply air were outdoor air, nearly that amount of airborne infectious particles might be wearied. However, conditioning that amount of outdoor air would be cost prohibitive and therefore considered out of the question.
Filtration
The combination of filtration equipment and airflow rates are often misunderstood or underappreciated for the effect they accept on the concentration of infectious agents in any conditioned space. Filtration should be considered healthcare's showtime line of defence force against infectious agents as it removes a large pct of them with every complete air change through an air handler. If the filter efficiency and/or air change rate is increased, a larger number of infectious agents would be removed per pass.
Therefore, it's important to view the return air and filtration system as a removal method of space generated contaminants - and not the air distribution side as a pathogen source, with the possible exception of some smaller viral particles. If at that place is concern hither, the application of UV-C in the air handler equipment is warranted.
Current design guidelines propose air change rates upwardly to 25 (upwardly to five of them as outdoor air) for new facilities, depending on the space served. Because most of the airborne pathogens originate from patients and room occupants, increasing the rates of supply air above design guidelines volition bring diminishing returns. Thus, the incremental benefit in preventing cross-manual is much more hard to demonstrate beyond 25 ACH. This can be seen in this uncomplicated equation:
Concentration (particles/cu.ft)=generation charge per unit (no. of people/action)
cfm ten filter eff. (removal charge per unit)
If either the cfm or filter efficiency is increased, the particle concentrations volition subtract mathematically. However, the algorithm favors reducing in-room source or generation rates of infectious agents, often referred to every bit source control or source reduction.
Pressurization
Pressurization protects against cross contamination from the infiltration of air from one space type to that of another. This is of great importance in healthcare settings, but information technology is very difficult to command. Frequently opened or propped open doors are all likewise mutual making corridors, etc., a conduit of contaminated air to other spaces. Although ORs and other areas are designed to be under positive pressure with respect to external spaces, this may not be the case when an air handler's airflow has been compromised!
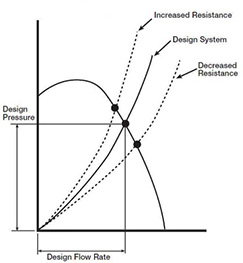
Note that air handler design resistance is the sum of all pressure losses through the system, including elbows, dampers, filters and coils, etc. The shape of a resistance curve will change when force per unit area losses change (Greenheck 1999). For instance, as filter resistance increases, organization air volume is reduced. But, like the filter, it's also common for the gyre pressure drop to increment, even double, which will result in a higher arrangement pressure drop too. The curves testify that equally the system's total resistance increases, air book and system pressure capability are reduced (at a constant fan RPM). This reduction in 'design-pressure' occurs oft today from reduced coil cleaning procedures, but its result is not at all obvious, and it's non only a reduction in air book, although that's important, it'southward also a reduction in relative room pressure capability! When i space is said to be negative in relation to other spaces, information technology assumes that the adjoining spaces are all 'positive'. A college curl pressure drop volition potentially negate that and permit the infiltration of contaminated air.
Measuring the pressure drop across a whorl and comparison information technology to as-built design data, or better, the manufacturer'south coil performance data, is one manner to determine a potential loss in airflow. If the curl pressure level drop is higher, the actual airflow should be measured to confirm that it matches as-built criteria. If the coil is fouled (common) and air force per unit area compromised, the 2011 ASHRAE Handbook – HVAC Applications recommends the installation of UV-C lamps to clean the ringlet and go on it clean continuously. A clean coil will assure proper airflow and pressure relationships with the added benefit of restoring equally-built cooling chapters (i.east., the heat-transfer characteristics). According to ASHRAE, UV-C will besides eliminate the growth of coil plenum mold and leaner removing the possibility of microbial products carryover and transfer to conditioned spaces.
Disinfection
In addition to opening and propping open of doors as a contaminant transfer way, the inbound and exiting of people likewise provides a contaminant source. It's known that the concentration of airborne bacteria is proportional to the number of personnel in the room (Mangram et al. 1999, Duvlis and Drescher 1980, Moggio et al. 1979, Kundsin 1976). The corporeality of surface contagion is also related to airborne contagion from occupation and action since these microbes settle continuously. The World Health System (WHO 1998) recommends a limit of 100 cfu (colony forming units)/m3 for bacteria and 50 cfu/m3 for fungi for sensitive areas. There are no published cfu standards in the U.Southward.
While the use of UV-C equipment, or disinfection, to control infectious agents in healthcare settings is one of its oldest uses, today the engineering is under-utilized. In the past seventy years it has used to disinfect upper air, ventilation air, and to sterilize medical equipment and water, with measured and successful results. Nonetheless, its utilise waned as dependence on antibiotics began in the tardily 1950s and beyond. UV-C destroys all microorganisms… and its use is extremely simple and cheap, but like all controls, information technology solitary is non a consummate answer.
UV-C for infection command
There are iii primary means of applying UV-C systems against infectious agents: upper-air (upper-room), coil irradiation, and airstream disinfection. Upper-air systems are installed in room spaces, such as above patient beds and in waiting rooms, corridors and break areas, etc. Roll irradiation and airstream disinfection systems are installed inside air handling units or duct runs. Upper room and HVAC applications are described beneath.
Upper Air/Room
The primary objective of upper-air UV-C placement is to interrupt the transmission of airborne infectious diseases in patient rooms, waiting rooms and other known microbial pathways such as lobbies, stairwells, laundry chutes, and emergency entrances and corridors, all of which can be effectively and affordably treated with UV-C (ASHRAE 2011). Airborne droplets containing infectious agents tin remain in room air for vi minutes and longer. Upper Air UV-C fixtures can destroy those microbes in a matter of seconds. Operating 24 hours a day, upper-air systems are as well especially effective at notably reducing the potential viability of surface microbes that settle out of room air.
Humans are the source of airborne agents which infect people (Nardell and Macher: ACGIH 1999). Again, upper-air systems intercept microbes where they are generated, thereby controlling them at the source (First et al. 1999). They have been shown to be effective against viruses and bacteria, including chickenpox, measles, mumps, varicella, TB, and cold viruses. Studies of Mycobacterium tuberculosis take shown that they tin can exist equivalent to x–25 air changes per hour (CDC 2005). In a study past Escombe et al. (2009), guinea pigs were exposed to frazzle air from a TB ward, of which 35 percent of the controls developed TB infections while simply ix.v percentage developed infections where upper air UV-C was used, yielding a decrease of 74 percent in the infection rate.
Measles and influenza viruses and the tuberculosis bacteria are diseases known to be transmitted by means of shared air between infected and susceptible persons. Studies signal that in that location are two transmission patterns: (I) within-room exposure such every bit in a congregate space; (II) transmissions beyond a room through corridors, and through entrainment inside ventilation ductwork where air is so recirculated throughout the building. Since the 1930s (Wells 1955; Riley and O'Grady 1961) and standing to the present day (Miller et al. 2002; Xu et al. 2003; First et al. 2007), numerous experimental studies take demonstrated the efficacy of upper-air UV-C. In add-on, effectiveness has been shown for reducing measles transmission in a school, and influenza transmission within a hospital (McLean 1961). What's more, newer fixtures bachelor today provide more than output and coverage at less cost and power. They likewise apply inexpensive and commonly available lamps!
HVAC systems
HVAC systems provide an fantabulous growth expanse for mold and some bacteria in and effectually cooling coils; drain pans (Levetin et al. 2001), plenum walls and filters. Growth of these microbial deposits likewise leads to curl fouling which will increment coil force per unit area drop and reduce airflow and heat substitution efficiency (Montgomery and Bakery 2006). Equally performance degrades, then does the quality, amount and pressurization capability of air supplied to conditioned spaces (Kowalski 2006/2009).
Because hospital codes telephone call for high-efficiency filters to exist located downstream of the cooling roll, they can also become damp and oftentimes moisture from saturated air there. Every bit such, air filters are considered a growth medium for mold and bacteria and an infectious-disease amanuensis reservoir. ASHRAE recommends UV-C lighting to exist installed downstream of the cooling roll; and then if a 360 caste UV-C system is installed in that location, it volition disinfect both the coil and the filter to destroy all microbes in and upon both devices. Information technology should also be noted that when using a 360-degree lamp in a "common" coil-irradiation system, it will besides kill infectious diseases in the airstream. For example, up to a 35 percent impale ratio of many infectious agents is achieved, thus providing a measurable increase in the combined removal rate of the two devices (Kowalski 2009).
UV-C design guidance
Chiefly, science has non found a microorganism that is resistant to the destructive furnishings of the 254-nm germicidal wavelength, including superbugs and all other microbes associated with HAIs. The question so – how are UV-C systems sized and practical?
Historically, engineers and facility practitioners wanting to use UV-C lacked specific guidance for systems design, sizing and specifications. ASHRAE undertook the process by forming a technical committee (TC ii.9 Ultraviolet Air and Surface Handling) to author capacity in their 2008, 2011, and 2012 ASHRAE Handbooks, which have been referenced herein. HVAC trade publications have also published several technical articles to assistance provide additional design guidance; these articles are cited in the sidebar, Technical Articles for Engineers. In total, these articles provide all practitioners with the guidance needed to successfully design, install, operate, and maintain successful UV-C applications in HVAC systems.
UV-C at large
UV-C's rising popularity beyond ASHRAE has also generated research by lesser-known organizations, such equally the Air Purification Consortium (APC); the Air Cleaning Industry Expert Advisory Panel (ACIEAP); and The National Center for Energy Management and Building Technologies (NCEMBT). UV-C energy has been crucial to achieving each of their goals, whether to save free energy, reduce biological contagion and maintenance or to reduce absenteeism. Their members are involved in high-stakes projects such as Homeland Security where application of UV-C is a crucial defense force against bioterrorism.
Condom & handling
Opening air handler doors to fan sections must exist minimized because it allows unfiltered air to enter and be dispersed to potentially sensitive areas, and/or information technology will disrupt pressure level relationships in the spaces served past them. Shutting these systems downwardly can also disrupt pressure relationships beyond the spaces served. Both of these functions, when necessary, should be coordinated with flooring nurses so that all room doors may exist closed before hand. Exposing filter surfaces to UV-C is an effective manner to destroy microbes on media surfaces. Nevertheless, constructed media filters are not compatible with UV-C while filters with glass media are. Caution should also be exercised when using unsupported "handbag" style filters every bit they inherently collapse when being replaced to expel potentially microbe- laden contamination. The CDC likewise recommends that all used filters be bagged upon removal to foreclose dispersion of microbial contagion during ship.
Where installed, facility staff should be trained how to inspect UV-C systems to ensure they are working properly. Controls should be installed to turn UV-C systems off when air-handler doors are opened. Centre and skin protection are needed to prevent exposure to UV-C lite when working in any area where the lamps are on.
UV-C lamps are very similar in construction to fluorescent lamps, and therefore contain trace amounts of mercury. The use of encapsulated lamps is recommended to prevent air-handler contagion should lamp breakage occur. Like fluorescent lamps, UV-C lamps should be replaced and recycled annually in a scheduled fashion.
Decision
UV-C installations are a simple, effective, and relatively cheap means of reducing concentrations of airborne and surface pathogens that cause healthcare associated infections. Within patient rooms, waiting rooms, and other congregational areas, upper-air UV-C units will kill airborne microorganisms that inherently circulate into the path of the UV-C light. UV-C lamps can be installed within HVAC systems downstream of cooling coils to continue coils make clean and to provide supplemental kill ratios in airstreams and on filter surfaces. Recent guidance from ASHRAE and published technical articles in HVAC trades provide healthcare engineers and facility staff with the resources needed to size, select, install, operate, and maintain UV-C systems.
Design considerations
• Concentration of airborne infectious agents is directly related to people activity
• Humans are the source of drug resistant microorganisms that effect humans
• Airborne transmission of infectious agents may exist more prevalent than proven
• UV-C inactivates and destroys microorganisms rendering them harmless
• seventy+ twelvemonth old Upper Air UV-C technology is heavily researched and proven effective
• Newer Upper Air UV-C units are more affordable and much more effective
• At six ACH an droplets of infectious agents tin can stay airborne for 10 minutes
• Upper Air UV can inactivate airborne infectious agents in a thing of seconds
• Source management will always prove to be the most effective means of control
• Increased ringlet pressure drib volition lower organisation airflow and space pressurization
• Bathing coils with UV-C cleans them, improves airflow and heat transfer efficiency
Additional Tips
• Install UV-C on cooling coils and drain pans to kill mold and restore airflow
• Manage room pressure relationships, especially during visiting hours
• Review and manage all air handler service, particularly filters and change-outs
• Manage air handler shutdowns, access door openings and coil pressure drop
• Install newer mode upper air UV-C fixtures in all spaces known for HAI's
• Also install them in corridors and waiting rooms connected to these areas
• Once airflow is restored, upgrade air filters and efficiencies where possible
Forrest Fencl is the president of UV Resources, Santa Clarita, Calif. He can be reached at forrest.fencl@uvresources.com.
ACGIH. 1999. Bioaerosols: Assessment and command, Ch. 9: Respiratory infections—Manual and ecology control, by E.A. Nardell and J.Thousand. Macher. American Briefing on Governmental Industrial Hygienists, Cincinnati, OH.
Allen K, Green H. 1987. Infirmary outbreak of multi-resistant Acinetobacter anitratus: An airborne mode of spread? J Hosp Infect 9:110–119.
ASHRAE, 2011 Handbook – HVAC Applications, Affiliate 60 – ULTRAVIOLET AIR AND SURFACE Treatment. Atlanta, GA.
CDC. 2005. Guidelines for preventing the transmission of Mycobacterium tuberculosis in health-care settings. Morbidity and Mortality Weekly Report (MMWR) 37-38, seventy-75.
Duvlis Z, Drescher J. 1980. Investigations on the concentration of air-borne germs in conventionally air-conditioned operating theaters. Zentralbl Bakteriol [B] 170(1–ii):185–198.
Escombe, A.R., R.H. Gilman, M. Navincopa, E. Ticona, B. Mitchell, C. Noakes, C. Martínez, P. Sheen, R. Ramirez, West. Quino, A. Gonzalez, J.S. Friedland, and C.A. Evans. 2009. Upper-room ultraviolet lite and negative air ionization to prevent tuberculosis transmission. PLoS Med 17(half dozen).
Farrington M, Ling T, French G. 1990. Outbreaks of infection with methicillin-resistant Staphylococcus aureus on neonatal and burns units of a new infirmary. Epidem Infect 105:215–228.
First MW, Nardell EA, Chaisson West, Riley R. 1999. Guidelines for the application of upper-room ultraviolet germicidal irradiation for preventing transmission of airborne contagion – Part II: Blueprint and operational guidance. ASHRAE J 105:869–876.
Beginning, M.W., F.M. Rudnick, K. Banahan, R.L. Vincent, and P.W. Brickner. 2007a. Fundamental factors affecting upper-room ultraviolet germicidal irradiation—Part i: Experimental. Journal of Environmental Wellness 4: 1-eleven.
Fletcher LA, Noakes CJ, Beggs CB, Sleigh PA, Kerr KG. 2003. The Ultraviolet Susceptibility of Aerosolised Microorganisms and the Role of Photoreactivation. Vienna: IUVA.
GREENHECK, 1999 – Production Application Guide, Fan Application No. FA/100-99
Kowalski, W.J. 2006. Aerobiological technology handbook. McGraw-Hill, New York.
Kowalski, Due west. 2009. Ultraviolet germicidal irradiation handbook. Springer-Verlag, Berlin.
Kundsin R. 1976. Operating Room as a Source of Wound Contagion and Infection. National Research Council, National Academy of Sciences, pp. 167–172.
Levetin, E., R. Shaughnessy, C. Rogers, and R. Scheir. 2001. Effectiveness of germicidal UV radiation for reducing fungal contagion within air-handling units. Applied and Environmental Microbiology 67(8):3712-3715.
Mangram AJ, Horan TC, Pearson ML, Silver LC, Jarvis WR, HICPAC. 1999. Guideline for prevention of surgical site infection. Am J. Infect Control 27(2): 97–132.
McLean R. 1961. The consequence of ultraviolet radiations upon the manual of epidemic influenzain long-term infirmary patients. Am Rev Resp Dis 83:36–38.
Moggio Chiliad, Goldner JL, McCollum DE, Beissinger SF. 1979. Wound Infections in Patients Undergoing Full Hip Arthroplasty. Ultraviolet Light for the Control of Airborne Bacteria. Arch Surg 114(7):815–823.
Montgomery, R. and R. Baker. 2006. Written report verifies gyre cleaning saves energy. ASHRAE Periodical 48(11):34-36.
Riley, R.50. and F. O'Grady. 1961. Airborne infection—Transmission and Command. Macmillan, New York.
R M Ryan, G E Wilding, R J Wynn, R C Welliver, B A Holm, C L Leach. Upshot of enhanced ultraviolet germicidal irradiation in the heating ventilation and air-conditioning system on ventilator associated pneumonia in a neonatal intensive care unit. Periodical of Perinatology accelerate online publication 24 March 2011; doi: ten.1038/jp.2011.16
WHO. 1988. Indoor air quality: Biological contaminants. Copenhagen, Kingdom of denmark: Earth Health Organization. Report nr European Series 31.
WHO. 1999. Guidelines for the Prevention of Tuberculosis in Health Intendance Facilities in Resource Limited Settings. Geneva: World Health Organization. Report nr WHO/CDS/TB/99.269.
Weinstein, RA, 2004. Planning for Epidemics — The Lessons of SARS. NEJM 350(23):2332-2334.
Wells WF. 1938. Air-borne infections. Modern Hosp 51:66–69. 232 ix Upper Room UV Systems
Wells WF, Wells MW, Wilder TS. 1942. The ecology control of epidemic contagion; I – An epidemiologic study of radiant disinfection of air in day schools. Am J Hyg 35:97–121.
Wells WF. 1943. Air disinfection in day schools. Am J Pub Wellness 33:1436–1443.
Wells WF. 1955. Airborne Contamination. Sciences AotNAo, editor. New York: New York University of Sciences.
Xu P, Peccia J, Fabian P, Martyny JW, Fennelly KP, Hernandez K, Miller SL. 2003. Efficacy of ultraviolet germicidal irradiation of upper-room air in inactivating airborne bacterial spores and mycobacteria in full-scale studies. Atmos Environ 37:405–419.
Source: https://www.healthcarefacilitiestoday.com/posts/Hospital-infection-control-reducing-airborne-pathogens--5523
Posted by: duvalldifors.blogspot.com


0 Response to "How Do Hospitals Keep Their Air Clean"
Post a Comment